Neck and Shoulder Pain
Have I got a ‘Frozen Shoulder’?
Frozen Shoulder, also called Adhesive Capsulitis, is a painful condition which results in a severe loss of motion in the shoulder. It may follow an injury, or it may arise gradually with no injury or warning. It most commonly affects patients between the ages of 40 to 60 years old and is twice as common in women as in men.
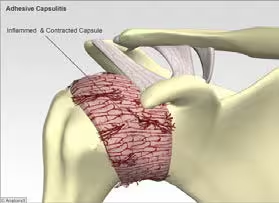
The shoulder is made up of three bones: the scapula (shoulder blade), the humerus (upper arm bone), and the clavicle (collarbone). The joint capsule is a sac that encloses the joint and the fluids that bathe and lubricate it. The walls of the joint capsule are made up of ligaments. Ligaments are soft connective tissues that attach bone to bone. The joint capsule has a considerable amount of slack, loose tissue, so the shoulder is unrestricted as it moves through its large range of motion. In frozen shoulder, inflammation in the joint makes the normally loose parts of the joint capsule stick together. This seriously limits the shoulder’s ability to move, and causes the shoulder to freeze. The cause of frozen shoulder is largely a mystery. One theory is that it may be caused by an autoimmune reaction. In an autoimmune reaction, the body’s defense system, which normally protects it from infection, mistakenly begins to attack the tissues of the body. This causes an intense inflammatory reaction in the tissue that is under attack. Frozen shoulder may begin after a shoulder injury, fracture, or surgery. Other shoulder problems like bursitis, rotator cuff tears, or impingement syndrome can lead to a frozen shoulder.
Symptoms
How is it treated?
Treatment of frozen shoulder can be frustrating and slow. The aim is to decrease inflammation and increase the range of motion of the shoulder. Osteopathic treatment is a critical part of helping you regain the motion and function of your shoulder. Treatments are directed at getting the muscles to relax using techniques to stretch the joint capsule and muscle tissues of the shoulder. You will also be given exercises and stretches to do as part of a home program. Your doctor may also recommend an injection of cortisone to get the inflammation under control. Cortisone is a steroid that is very effective at reducing inflammation but cannot be used continuously. If you fail to respond your doctor may offer you the option of manipulation under anaesthetic.
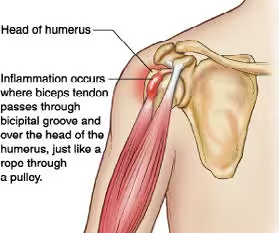
Biceps Tendonitis
Fortunately, biceps tendonitis and rotator cuff problems are more common than frozen shoulder and with treatment, usually resolve more quickly.
Symptoms
Patients generally report the feeling of a deep ache directly in front of and on top of the shoulder. The ache may spread down into the main part of the biceps muscle. Pain is usually made worse with overhead activities. Resting the shoulder generally eases the intense pain but aching and discomfort may persist. The arm may feel weak with attempts to bend the elbow or when twisting the forearm into supination (palm up). A catching or slipping sensation felt near the top of the biceps muscle may suggest a tear of the transverse humeral ligament.
Treatment for biceps tendonitis has similarities to that of frozen shoulder and is directed at reducing the inflammation and pain, increasing the range of movement and gradually strengthening the shoulder with directed home exercise. Hot and cold therapy as described in previous articles helps to reduce pain and promote healing.